Background
Recently, FDA approved the dual immunotherapy treatment for hepatocellular carcinoma with Astrazeneca’s Imjudo (tremelimumab) combined with Imfinzi (durvalumab), marking the second time of this year for the authoritative approval of dual immunotherapy for the treatment of cancer. The first dual immunotherapy treatment for cancer came on March 18, when FDA approved Bristol-Myers Squibb’s OpdualagTM (nivolumab and relatlimab-rmbw) to treat unresectable or metastatic melanoma.
Antibody is undoubtedly the main force in the treatment of tumors by immunotherapy including double immunotherapy. However, antibody has the disadvantages of hig cost and poor oral applicability. Fortunately, peptide-based drugs with much smaller molecular weight than antibodies could overcome the limitations and play a significant role in immunotherapy against tumors.
Peptides have a small size, high affinity, and low immunogenicity, and are easy to modify. Some modified peptides showed excellent stability, such as the antibody proteins in the two dual immunomodulators above. Peptide molecules can act as immune checkpoint inhibitors in tumor immunotherapy. Instead of attacking tumor cells directly, immunotherapy drugs modulate the patient’s immune system and attack tumor cells by targeting immune checkpoints.
What is immune checkpoint?
When proteins on the surface of T cells recognize and bind to companion proteins on other cells, immune checkpoints work. The proteins on these T cells are called immune checkpoints. When the checkpoints bind to the cancer cell’s chaperone proteins, they will send an “off” signal to the T cell. Immune checkpoint molecules matter a lot in the immune escape of tumors and can be used to restore the anti-tumor function of immune cells by blocking the binding of immune checkpoints and ligands in the clinic, so as to achieve the purpose of tumor treatment.
Since immune checkpoints can prevent overactive immune responses and sometimes hinder T cells from killing cancer cells, when these checkpoints are blocked or inhibited, T cells are better able to kill cancer cells. This result can bring a very positive effect on tumor therapy. Therefore, immune checkpoints can act as targets for cancer immunotherapy because they have the potential to be used in the treatment of many types of cancer.
Examples of checkpoint inhibitors
Currently approved checkpoint inhibitors are used to block CTLA4, PD-1, and PD-L1.
- CTLA4 inhibitors
CTLA-4 or CTLA4 (Cytotoxic T lymphocyte antigen-4), also known as CD152, is a protein receptor that acts as an immune checkpoint and downregulates immune responses. CTLA-4 is expressed in regulatory T cells but only upregulated in conventional T cells after activation. This phenomenon is particularly evident in cancer.
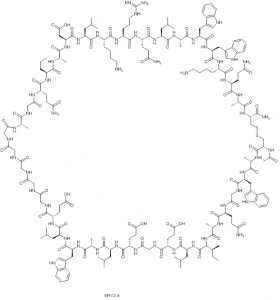
mAb antibody inhibitors that target the immune checkpoint CLTA4 include ipilimumab for melanoma. Many active peptides also showed a good inhibitory effect on CTLA4. For example, yeast-displayed peptide ERY2-4 specifically bound to CTLA-4 with a KD of 196.8 ± 2.3 nM. Furthermore, ERY2-4 blocked the interaction between CTLA-4 and dendritic cells (DCs) presenting B7 on their surface. Importantly, ERY2-4 showed no cross-reactivity against CD28, suggesting it does not suppress T-cell activation. Since CTLA-4 is a critical immune checkpoint for restricting the cancer immune response, this inhibitory peptide represents a new class of drug candidates for immunotherapy.
Fig1. The structure of yeast-displayed peptide ERY2-4
- PD-1
Although PD-1 and CTLA-4 belong to the CD-28 immune checkpoint receptor family, their roles in suppressing the immune response are mechanistically different. CTLA-4 regulates immune response mainly in lymph nodes in the early stage, while PD-1 regulates immunosuppression in peripheral tissues in the later stage. Nevertheless, clinically approved antibodies against both pathways produced long-lasting clinical responses, they both resulted in adverse consequences and anti-CTLA-4 antibodies showed a higher incidence and level of immune-related adverse reactions. The better clinical profile of PD-1/PD-L1 checkpoint inhibitors in terms of efficacy and safety has led to rapid drug development and approval in multiple indications. In this area, Bristol-Myers Squibb has patented their cyclic peptide, which has been shown to have nanomolar activity in inhibiting PD-1/PD-L1 interactions.
- BTLA-4
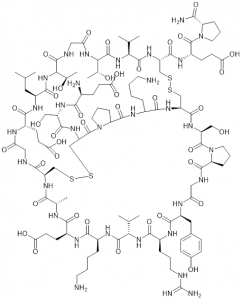
B and T lymphocyte attenuation factor (BTLA) is another co-inhibitory receptor in the CD-28 family. In a recent report, based on the natural protein HVEM (herpesvirus entry mediator), which binds to BTLA, researchers designed a disulfide bond bridging peptide using the HVEM (14-39) fragment. BTLA expressing 293T cells were used to demonstrate their cellular activity. HVEM (14 — 39) peptide is a BTLA/HVEM binding inhibitor that inhibits the formation of BTLA/HVEM complex in a dose-dependent manner. It deserves further development in the field of immunotherapy against tumors.
Fig2. The structure of HVEM (14-39) peptide
- VISTA
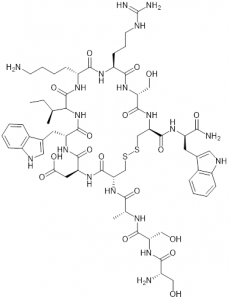
VISTA is an immune checkpoint in the B7 family that collaborates with the PD-1 protein to regulate T-cell responses. CTLA-4 and PD-1 inhibit immune function during T-cell initiation and effect, while VISTA inhibits immune response during the earliest stages of T-cell activation. To this end, the researchers designed VISTA peptide antagonists. This is a cyclic peptide containing a disulfide bond and multiple D-amino acid residues.
Fig3. VISTA peptide inhibitor
The peptide VISTA antagonist significantly enhanced T cell proliferation compared with anti-VISTA antibody or anti-PD-L1 antibody. In addition, the antitumor efficacy of this VISTA antagonist peptide was demonstrated in a model of immunogenic bladder cancer MB49. The founding suggests that the mechanism of action may be that peptides bind to key/active sites in VISTA, thereby blocking VISTA’s immunosuppressive function.
- LAG-3
LAG-3 is the third clinically targeted immune checkpoint receptor after CTLA-4 and PD-1. LAG-3 is co-expressed with other receptors, especially PD-1, and inhibits immune function in a variety of settings, making it an attractive target for combination with PD-1. The anti-LAG-3 and anti-PD-1 antibodies have been a success in the treatment of melanoma. Bristol Myers Squibb’s OpdualagTM, whose active ingredients nivolumab and relatliab-RMBW are antagonists of PD-1 and LAG-3, respectively, was approved by the FDA on March 18, 2022. OpdualagTM thus became the first immunotherapy targeting LAG-3 approved by the FDA.
In the study of peptide LAG-3 antagonists, researchers designed a disulfide cyclic peptide named C25, which has a KD value of mM and can effectively bind to LAG-3, thus efficiently interfere with the binding between LAG-3 and MHC-II (major histocompatibility complex protein II).
Conclusion
Immune checkpoint antagonists are currently dominated by antibodies, but low response rates and immune-related adverse consequences require the development of more effective and safer therapeutic modalities. Peptide drugs have potential advantages in selectivity, efficacy, and reduction of off-target toxicity. In the future, peptide immunotherapy may lead to the development of parallel antibody drugs, and perhaps peptide dual immunotherapy similar to OpdualagTM.
Related Products:
| Product | Description |
| Checkpoint Inhibitors | Checkpoint inhibitors are also described as a monoclonal antibody or targeted therapy. |
| Therapeutic Peptides | Therapeutic peptides are a unique class of pharmaceutical agents composed of a series of well-ordered amino acids. |
| Peptide Inhibitors | Peptide inhibitors have the advantages of high affinity and specificity, low production cost, etc., and have attracted the attention of researchers. |
Related Services:
| Service | Description |
| Pharmaceutical Peptides Services | The pharmaceutical peptides services of Creative Peptides can help you significantly shorten the development time of peptide drugs in the development of peptide drugs. |
References
- Tharanga, M. R. et al. An Immune-Stimulatory Helix–Loop–Helix Peptide: Selective Inhibition of CTLA-4–B7 Interaction. ACS Chem. Biol. 2020,15, 360–368.
- Callahan, M. K. At the bedside: CTLA-4- and PD-1-blocking antibodies in cancer immunotherapy. J Leukoc Biol, 2013, 94, 41-53.
- Liu, J. et al. Immune-checkpoint proteins VISTA and PD-1 nonredundantly regulate murine T-cell responses. Proc. Natl. Acad. Sci. U.S.A. 2015, 112, 6682-6687.