Diabetes mellitus (DM) is a group of metabolic diseases classified by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Diabetes is prevalent worldwide and the number of patients is drastically rising, with a predication of 366 million in 2030 due to factors such as obesity, inactivity, aging, and hormonal disorders. While there are many available treatment regimens for type 2 diabetes, some of the older therapies can cause undesirable adverse events, including hypoglycemia, hunger and weight gain. The latter is particularly problematic as insulin resistance is strongly correlated with obesity. Some other related metabolic complications include cardiovascular disease and dyslipidemia, all resulting in an increased risk of mortality.
Introduction of GLP-1
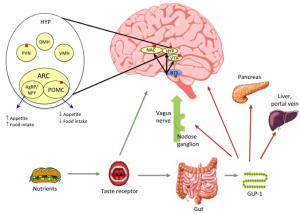
GLP-1 is a gastrointestinal peptide that stimulates glucose-dependent insulin release from pancreatic islets, slows gastric emptying time, inhibits inappropriate post-meal glucagon release, and ultimately reduces food intake. GLP-1 actions are mediated via the high affinity GLP-1 receptor. Impaired secretion of GLP-1 can contribute to type 2 diabetes. GLP-1 also induces satiety, resulting in lower voluntary caloric intake. These mechanisms together allow for significant blood glucose control and meaningful weight loss.
The advantages of GLP-1 drugs
Insulin therapy has a high risk of hypoglycemia, while GLP-1 is hypoglycemic in the form of glucose dependence, so the risk of hypoglycemia is extremely low. Most patients with type 2 diabetes are obese, and further weight gain associated with insulin injection can exacerbate metabolic disorders and diabetes-related complications (including microvascular and macrovascular complications). The weight loss effect of GLP-1 drug therapy is very beneficial to patients with diabetes. More importantly, its cardiovascular benefits provide excellent clinical compliance for long-term GLP-1 treatment.
The challenge of GLP-1 drugs
Compared with insulin, GLP-1 has a unique biological function, and its hypoglycemic effect can be changed according to the change of blood glucose level. Therefore, even by oral administration, the lack of pharmacokinetics of GLP-1 is no longer a major challenge compared with insulin. However, since patients with type 2 diabetes often need to take multiple drugs at the same time, the main challenges facing oral GLP-1 drugs are feeding and the potential dangers of drug-drug interactions. The ultimate success of oral peptides or recombinant protein drugs requires a large number of clinical studies and verification by real-world patients after launch. In addition, due to the very low bioavailability of oral preparations, an injection dose of more than 10 to 100 times is usually required. Its production cost and price are also key to determining whether the drug can be used by American insurers and the European health care system.
Conclusion
As GLP-1 drugs enter the ADA-EASD guidelines as first-line drugs for type 2 diabetes, there will be a great market demand for GLP-1 drugs. Long-acting human GLP-1 drugs have insulin-similar hypoglycemic effects. Not only extremely low risk of hypoglycemia, its weight loss and cardiovascular benefits will alleviate the long-term type 2 diabetic patients whom needs lifelong treatment. Factors such as patient self-care, the occurrence of complications, and the pressure to bear the cost of drug treatment over a long period of time will also play a part to impact the treatment outcome for patients.
In conclusion, the market needs diabetes drugs that are high-quality, low-cost, affordable, and have multiple effects to improve patients’ metabolic syndrome and quality of life. Long-acting human GLP-1 drugs will be the main force in the diabetes market in the future.
References
1. Kristensen, S. L., Rørth, R., Jhund, P. S., Docherty, K. F., Sattar, N., Preiss, D., … & McMurray, J. J. (2019). Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. The Lancet Diabetes & Endocrinology.
2. Hirsch, I. B. (2019). The Future of the GLP-1 Receptor Agonists. Jama, 321(15), 1457-1458.